What are some good revenue cycle management automation examples? How can they make a difference?
Many healthcare leaders, just like you, know there are big opportunities with technology to save time and work more efficiently. But who actually has the time to figure it all out and then implement it successfully? You know it can make your practice better—especially in the financial department—but where should you start?
It's a common dilemma these days. This is precisely why exploring revenue cycle management automation examples is so essential. Let's break this down and finally get you on the fast track to working smarter.
Why Revenue Cycle Management Matters - More Now Than Ever
In 2021, a forecast predicted the Revenue Cycle Management software industry was about to take off with an anticipated 10% annual growth rate from 2021 through 2025. This research demonstrates how rapidly the healthcare landscape is evolving - RCM software quickly transitioned from being "nice to have" to becoming an absolutely vital component of any efficient practice, billing department or hospital system.
But that doesn't mean there aren’t some holdouts. Just like paper charts still lurking in some dusty back rooms, some healthcare providers continue to depend on time-consuming and error-prone manual revenue cycle processes. These old methods are simply unsustainable and contribute to delays, errors, denials, and burnout.
By overlooking RCM automation, practices risk falling behind in today's digital-first environment, and their bottom line and patients will undoubtedly be the ones who suffer.
How Many Providers Still Rely on Manual Processes?
This is the real kicker. Shockingly, in 2020 it was found that a whopping 87% of providers were still stuck in the dark ages - using manual and paper-based systems for collections.
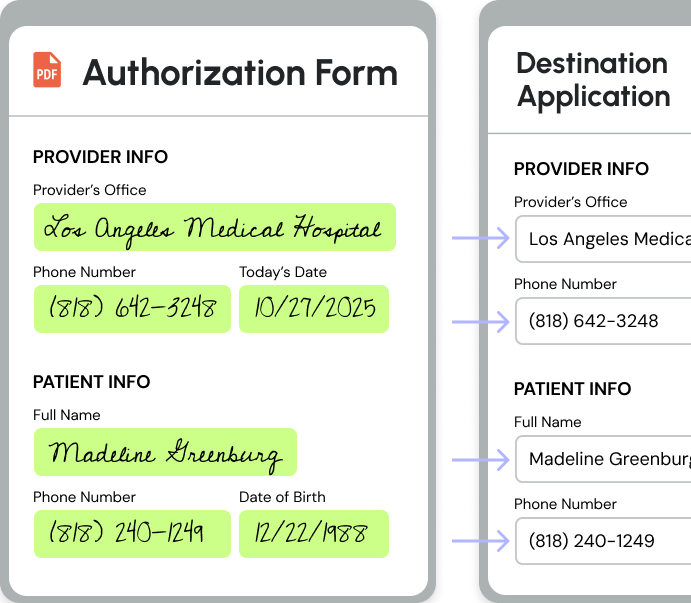
This is why more and more healthcare companies are turning to automation tools like Magical. Magical helps healthcare admin teams eliminate repetitive typing tasks like data entry and moving patient data between systems.
5 Real-World Revenue Cycle Management Automation Examples
Let's shift gears now and take a look at some stellar revenue cycle management automation examples currently in play and making big changes. These instances highlight the real-world applications of RCM automation across various aspects of a healthcare practice, billing department, and hospital system.
Remember, though, automation isn't simply a set-it-and-forget-it solution. To really maximize effectiveness, the human element must still play a vital role in overseeing, managing, and refining these automated processes:
1. Automated Patient Registration
North Kansas City Hospital improved digital patient registration and automated scheduling by deploying AI. This resulted in a fully digitized, automated registration experience, along with care gap outreach. The health system, which includes more than 140 primary and specialty care physicians across 30 locations, has been recognized as a Best Hospital in the Kansas City metro area and in Missouri.
After achieving 99.3% patient satisfaction and scheduling 80,000 appointments within three weeks of deployment, North Kansas City Hospital is expanding Intelligent Scheduling across primary and specialty care areas. Furthermore, the hospital saw a 70% digital completion rate and a 23% decrease in no-show rate. North Kansas City Hospital and Meritas Health's automated scheduling also drove a 2X increase in new patient appointments.
“By leveraging AI to match each patient with the correct provider, Intelligent Scheduling has increased provider adoption of online scheduling. We are excited to expand Intelligent Scheduling across primary and specialty care areas after achieving 99.3% patient satisfaction and scheduling 80,000 appointments within three weeks of deployment.”
- Kristen Guillaume, CIO, North Kansas City Hospital
2. Streamlined Claims Processing and Management
Did you know that errors can be found in as much as 80% of medical bills submitted to insurance? Sadly, nearly a quarter of all healthcare dollars—a staggering $125 billion annually—are gobbled up by improper payments, according to CMS. This is where RPA automation and automation tools can help.
AI-supported systems can improve hospital claims management by identifying and correcting errors, which benefits health insurers and providers. In Germany, where inpatient treatment costs amount to EUR 73 billion (30–40% of a typical health insurer's budget), 8–10% of claims are incorrect. By using intelligent algorithms that learn from historical cases, AI systems are proven to be able to save German health insurers an estimated EUR 500 million annually. These systems identify claims with a high likelihood of successful intervention and automate the processing of unobjectionable cases, allowing staff to focus on complex reviews.
The implementation of AI in claims management involves several steps: data compilation and preprocessing, data analysis, model development, results evaluation, and piloting. To ensure success, insurers need digitized original claims, an established claims management process, and structured documentation of results. A cognitive system, which emulates cognition to draw conclusions and make informed decisions, is central to this process. This leads to greater efficiency, valid decisions, and significant savings by focusing resources on relevant cases and reducing redundant processes.

3. Transforming Patient Billing and Collections
We are all busy. As much as we dislike being bombarded with automated payment reminders from the doctor's office, there are not enough hours in the day for staff to make these calls personally - let alone hunt down overdue balances. This is where technology truly excels.
RCM automation simplifies the collections process with secure payment gateways and easy-to-use platforms designed to send timely invoices (electronically) directly to the patient - either on a set schedule or as needed. But remember - personalized touches, even if automated, are vital. It all comes down to sending the correct messages to the right person at just the right time.
Atlas Health, for example, was able to implement AI to optimize their financial assistance programs so they could automatically match patients to eligible programs. (Atlas gets an estimated $30 billion in funding per year from a variety of 5013C foundations to cover such medical issues as complex diseases, high cost drugs and recurring procedures.) On average, Atlas saves health systems up to 0.4 - 0.7% of their net patient revenue using AI.
4. Effortless Denial Management and Resolution
Have you heard the saying, "an ounce of prevention is worth a pound of cure"? Well, this certainly rings true when we're discussing claim denials. It can take weeks—or even months—to iron out just a single denied claim and get this fully resolved with the correct payment finally received. It is crucial that the appeals process be tackled efficiently—and quickly.
Imagine though, not even having to deal with most denials. Just like in the scenario above, where claim errors are proactively corrected, automation streamlines this vital step in your revenue cycle by automatically flagging, challenging, and following through with denials.
This is the case at the University of Arkansas for Medical Sciences, where they have been using AI to automatically create strong appeals in a fraction of the time it would take manually using AI.
“At UAMS, we’ve seen how rising denials adversely affect our bottom line, which ultimately impacts our ability to invest more in patient care. With AI, we can create strong appeals in a fraction of the time, which is a gamechanger."
- Dr. Cam Patterson, CEO, University of Arkansas for Medical Sciences
5. RCM Agentic AI for Prior Authorizations, Eligibility Verifications, and More
Magical offers best-in-class agentic ai for revenue cycle management. Our team has successfully completed the certification from the HFMA to have one of its AI agents officially become a Certified Revenue Cycle Management Representative. You can use a Magical AI agent to easily automate tasks like prior authorizations because it uses adaptive intelligence to make decisions during an automation just like a human would.
Check it out:
FAQs About Revenue Cycle Management Automation Examples
How is AI Used in Revenue Cycle Management?
AI has the potential to dramatically transform the speed and accuracy of tasks in revenue cycle management, such as:
- Data entry.
- Claim submission.
- Insurance eligibility verification.
- Prior authorization.
- Billing.
- Payments.
- Patient collections.
- Reporting.
- Data analysis.
What Is Automation in the Revenue Cycle?
Revenue cycle management (RCM) automation involves incorporating software and technology to automate and optimize all the manual, repetitive administrative and financial tasks associated with the revenue cycle.
What Is RPA in Revenue Cycle?
In revenue cycle management (RCM), robotic process automation (RPA) utilizes software bots to automate tasks that have historically been handled manually.
What is revenue cycle management technology?
Revenue cycle management technology is software or a suite of applications that streamline the various aspects involved with processing patient claims. A fully integrated RCM system incorporates each phase of the process and begins when a patient schedules an appointment, continuing through claim submission to payment posting.
The Time For Automation in RCM Is Now
With these impressive revenue cycle management automation examples at your fingertips, it's easier than ever to envision how integrating intelligent technologies into your organization can be truly transformative for your medical billing process. By automating the laborious tasks that consume so much time and mental energy, not only will your bottom line reap huge rewards—but think of how happy and fulfilled your staff will be.
One of the tools you can add for your admin teams is Magical. Magical is used at more than 50,000 companies like Optum, Zoomcare, and Dignity Health to save 7 hours a week (on average) on their repetitive tasks. Try it for your team today!