Healthcare is a complex and ever-changing field. However, one thing remains constant: healthcare providers need to get paid for their services. This is where revenue cycle management for medical billing comes in. It's a critical process that ensures healthcare providers receive timely and accurate payments for the care they provide.
But sometimes RCM for medical billing can feel overwhelming. With so many moving parts and regulations to keep up with, it's easy to get lost in the details. Let's break it down and see how it works.
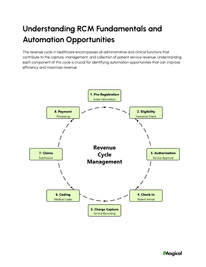
Understanding The Medical Billing Revenue Cycle
The revenue cycle is essentially the lifeblood of any healthcare organization. It is a multi-step process that starts when a patient schedules an appointment and ends when the healthcare provider receives payment. While this sounds straightforward, the billing process has potential pitfalls.
The Steps in Medical Billing Processes
While specifics may vary between different healthcare providers, the core elements of a robust revenue cycle management process generally follow a similar structure:
Patient Scheduling and Pre-Registration:
It begins when a patient calls to schedule an appointment. The staff will gather basic demographic data and insurance details.
Insurance Verification and Authorization:
Before the appointment, it is crucial to verify the patient's insurance coverage. This includes checking for eligibility, co-pays, deductibles, and pre-authorization requirements for certain procedures.
Patient Check-in and Documentation:
When the patient arrives for their appointment, staff should confirm all details are still correct and capture any necessary updates. This is also where essential documentation about the patient's visit begins, ensuring everything is tracked accurately.
Medical Coding:
After the appointment, trained coders will review the patient's chart and assign specific codes that represent the diagnoses, treatments, and procedures performed.
Claim Submission:
Using the medical codes, a claim is created and sent electronically to the insurance company for reimbursement.
Payment Posting:
After reviewing the claim, the insurer will issue payment (or a denial). Healthcare staff post these payments to patient accounts. This helps to ensure that they accurately reflect the money owed.
Denial Management:
Claims can sometimes be denied. Common reasons for denials include coding errors, missing information, or issues with the patient's insurance coverage.
Denial management involves figuring out why a claim was denied and fixing it. Then, the provider must appeal to the insurance company and resubmit the claim, to secure eventual reimbursement.
Editor's Note: Many of the errors that occur during registration or eligibility verification are due to data entry mistakes. Many companies in the healthcare industry like United Healthcare are turning to Magical to help with these errors.
Magical is an automation and productivity tool that eliminates repetitive typing tasks like patient registration and transferring patient data between systems. You can set up automations with Magical to autofill forms, thereby reducing errors and boosting revenue.
Patient Billing:
Once the insurer has paid their portion, the provider bills the patient for any remaining balance. This includes things like co-payments or costs for procedures not covered under their plan.
The Importance of Medical Billing and Coding Accuracy
For successful RCM, the steps of medical billing and coding need to be completed accurately. Assigning the wrong codes for diagnoses, procedures, or supplies can lead to claim denials and a delay in getting reimbursed. Errors are some of the biggest challenges in medical billing today.
Even worse, these errors might result in legal and financial penalties down the road. Medical billing processes must follow stringent rules.
Many organizations are opting to outsource these complex processes to improve patient satisfaction. By relying on the expertise of specialized teams, they reduce the chances of errors and streamline their financial flow.
Research indicates that this global revenue cycle management outsourcing market is steadily expanding, and the size is predicted to more than double from 2017 to the end of 2023. Clearly, healthcare providers recognize the value of having their billing and coding processes handled efficiently and with high accuracy.
Challenges Faced in Revenue Cycle Management for Medical Billing
Let's face it: managing the revenue cycle isn't always easy. Some things can make the process tougher and sometimes slow things down. This leads to financial stress, which isn't ideal for anyone involved.
Dealing with Claim Denials and Rejections
Claim denials are a significant problem in healthcare, representing a big source of revenue loss for healthcare organizations. While the majority of claims do eventually get approved for payment, industry sources estimate that initial denials affect somewhere between 5-25% of submitted claims. Handling these denials requires dedicated time and effort from billing staff, who must fix the denied claims.
Sometimes, appealing denials can turn into lengthy back-and-forth communication with the insurance companies. Healthcare providers are increasingly using accounts receivable to manage claim denials.
Navigating Complex Coding Systems
The healthcare field relies on complex medical coding systems, with countless codes for various procedures, diagnoses, and supplies. These codes are constantly being updated, making accurate billing a moving target. Medical professionals use systems like the ICD-10 and CPT codes to translate services provided into codes for claim submissions.
Staying on top of these changing regulations, interpreting guidelines, and using the codes correctly poses a considerable challenge. Staying informed about regulatory requirements and ensuring billing compliance is essential for healthcare providers to receive accurate reimbursement for their services. The ever-evolving nature of medical coding necessitates ongoing education and training for billing staff to avoid claim denials.
Balancing Patient Financial Responsibility
In recent years, we've seen a shift towards patients taking on more financial responsibility for their care. As high-deductible plans become the norm, it is more difficult to get paid in a timely manner.
Healthcare organizations must strike a delicate balance between collecting patient payments and maintaining positive patient experiences. Implementing patient-friendly billing practices, such as offering flexible payment options and providing clear explanations of bills, can improve patient satisfaction and reduce the risk of bad debt.
Biggest Benefits of Revenue Cycle Management Tools
When incorporating revenue cycle management (RCM) tools into your practice, you're opening the door to numerous benefits. These tools are designed to streamline the entire billing process, maximizing efficiency and minimizing the potential for errors. Let's delve into some of the key advantages:
1. Enhanced Operational Efficiency: RCM tools automate routine tasks such as data entry, insurance verification, and claim submission. This automation not only saves time but also reduces the likelihood of human error. With these efficiencies in place, your staff can focus on delivering quality patient care rather than getting bogged down by administrative tasks.
2. Increased Financial Performance: By optimizing processes and reducing delays in claims processing, revenue cycle management tools can significantly improve your practice's financial performance. You'll benefit from faster reimbursements and a decrease in claim denials, ensuring a more consistent cash flow.
3. Improved Patient Experience: Efficient RCM allows for smoother transactions, from patient patients to care scheduling to billing inquiries. Patients will appreciate accurate, timely billing, which can enhance their overall experience with your healthcare facility. Clear communication regarding their financial responsibilities is crucial, and RCM tools facilitate this transparency.
4. Comprehensive Analytics and Reporting: RCM tools offer advanced analytics and reporting features that provide actionable insights into your financial operations. By examining these analytics, you can identify trends, uncover bottlenecks, and make informed decisions to optimize your revenue cycle further.
5. Adaptability and Scalability: As your practice grows, your RCM tools can easily scale to accommodate increased patient loads and more complex billing scenarios. This adaptability ensures that your operations remain seamless irrespective of changes in volume or complexity.
Incorporating effective RCM solutions into your healthcare practice is not just about keeping up with the industry standards; it's about propelling your operations forward. By leveraging these tools, you can ensure your healthcare practice runs smoothly, remains profitable, and continues to provide exceptional care.
6 Strategies to Improve Your Medical Billing Revenue Cycle
If you feel overwhelmed by the complexities of the billing cycle, don't despair. Here are practical tips that any healthcare organization can implement to get a better handle on their finances. Using electronic health records (EHRs) can greatly enhance revenue cycle management by improving documentation accuracy, streamlining workflows, and facilitating electronic claim submissions.
1. Invest in Effective Technology and RCM Software
There's no doubt that the world of medical billing heavily relies on specialized software to manage and streamline operations. Look for software solutions that have features like automated eligibility verification, claims scrubbing, reporting, and patient portals.
Utilizing tools that let patients schedule appointments online, make payments, and view their statements can save a ton of time for your billing staff and also make things a whole lot easier for your patients. A smoother, easier process usually translates into fewer late payments.
2. Streamline the Patient Registration Process
Try to capture as much information from patients during scheduling and pre-registration. You can even provide them with the necessary forms online beforehand. Making this process as smooth and efficient as possible sets a positive tone for the patient's entire experience and minimizes errors later on.
3. Focus on Accurate Data Entry and Medical Coding
As previously mentioned, precise data and correct medical coding are essential to the revenue cycle. Invest in quality training programs for your staff who handle these processes and keep them informed about updates to codes and guidelines. Consistently audit claims to proactively spot errors.
4. Create a Proactive Denial Management System
Don't wait until denied claims start piling up. It is better to build a robust denial management process into your existing workflow.
Implement procedures for immediate action when denials occur, develop standard appeal letters that your billing staff can customize based on the type of denial, and look at the patterns in denial reasons to identify areas where training can reduce future issues. Prioritizing denial management is crucial for maximizing revenue and reducing write-offs.
5. Prioritize Patient Communication and Education
Clearly communicate your financial policies to your patients. Offer patients options for online bill pay and set up a patient portal where they can conveniently view and manage their bills. When your patients are in the loop and understand their financial responsibility, they are more likely to make payments promptly, minimizing any unnecessary delays or disputes.
Providing patients with the option to receive and pay their bills online through a secure patient portal can significantly enhance their financial experience. This convenience empowers patients to manage their healthcare expenses proactively.
6. Embrace Continuous Evaluation and Improvement
The world of healthcare billing and coding never stands still, so it's critical to make a regular practice of analyzing your RCM performance and making adjustments. Analyze denials to look for recurring reasons or departments experiencing problems and use that data to train staff on correcting those areas.
Track key performance indicators to spot where things might be slipping, such as a rising average collection period or an increasing volume of denied claims. Continuously improving can only happen when you commit to analyzing what works well and what could use some fine-tuning. Regularly evaluating and optimizing your revenue cycle management processes is essential for adapting to the dynamic healthcare landscape and maximizing financial performance.
Final Thoughts
Revenue cycle management for medical billing is more than just about getting paid, it's about having a well-oiled system. The overall financial well-being of any healthcare organization hinges on effective RCM. That requires attention to detail, ongoing training, adaptability, and willingness to make adjustments.
If you're part of a healthcare organization and want to know how to manage patient data and other administrative tasks more efficiently, try Magical. Magical is used at more than 50,000 companies like Dignity Health, Optum, and Zoomcare to save 7 hours a week on their repetitive tasks.


.webp)